
WALKING DISTURBANCE
BODY MECHANISM
COMMON PATHOLOGICAL GAITS
AND PHYSIOTHERAPY ROLE IN GAIT TRAINING
NORMAL WALKING PATTERN
NORMAL WALKING PATTERN / GAIT CYCLE
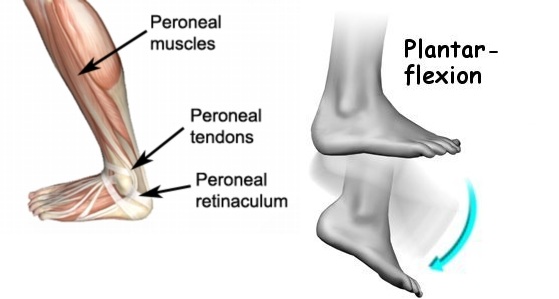
During a normal gait pattern, the knee extends such that the lower leg swings forward with the foot flexed and raised upward (dorsal flexion) in order to clear the ground. The leg is then extended and the body moves forward, resulting in a heel strike of the foot followed by an extension of the foot (plantar flexion) as the foot is placed down on the floor. This is followed by the “toe off” phase of gait where the heel of the foot starts to raise during the push-off phase of gait.

The patient is unable to flex the hip and shortens the step length during the swing. The compensatory mechanism adopted by the patient will be a backward thrust of the trunk with circumduction, lateral trunk movement towards the side with elevation of the hip on the affected side or hip hiking.
2. Weakness of hip abductors:
Dropping of the pelvis on the opposite side with lateral flexion of the trunk and head on the affected side. This is known as Trendelenburg or gluteus medius dip gait.

Compensated gluteus medius gait:
Here the gluteus medius weakness is compensated by the medial deviation of the hip on the affected side. The trunk bends sideways on the affected hip on weight-bearing, and the opposite hip is lifted up for the clearance of the ground. In the presence of limb length disparity, the patient has similar tendency which needs to be rectified by limb length measurement and manual muscle test.
3. Weakness of hip extensors:
In gluteus maximus gait, following heel strike of the affected leg, jerky backward thrust of the trunk occurs with simultaneous protrusion of the affected hip. Backward thrust of the trunk keeps the CoG behind the hip joint to counteract the inertia produced by the forward movement of the trunk. At midstance, the knee is held in extension.
Exaggeration of lumbar lordosis: During the stance phase, the gait may suggest hip flexion contracture on the side of the stance leg. Persistent inclination of the pelvis, to one side during all the phases of gait cycle, combined with lack of heel strike suggests an adduction contracture on the side of the inclination.

4. Weakness of quadriceps:
There is forcible extension on the knee at heel strike. This is done by using ‘hand support on thigh’ position at midstance, knee can be drawn backward by hip extensor as well as by gastro-soleus on weight bearing by producing equinus foot. Unprotected repeated extension may result in genu recurvatum

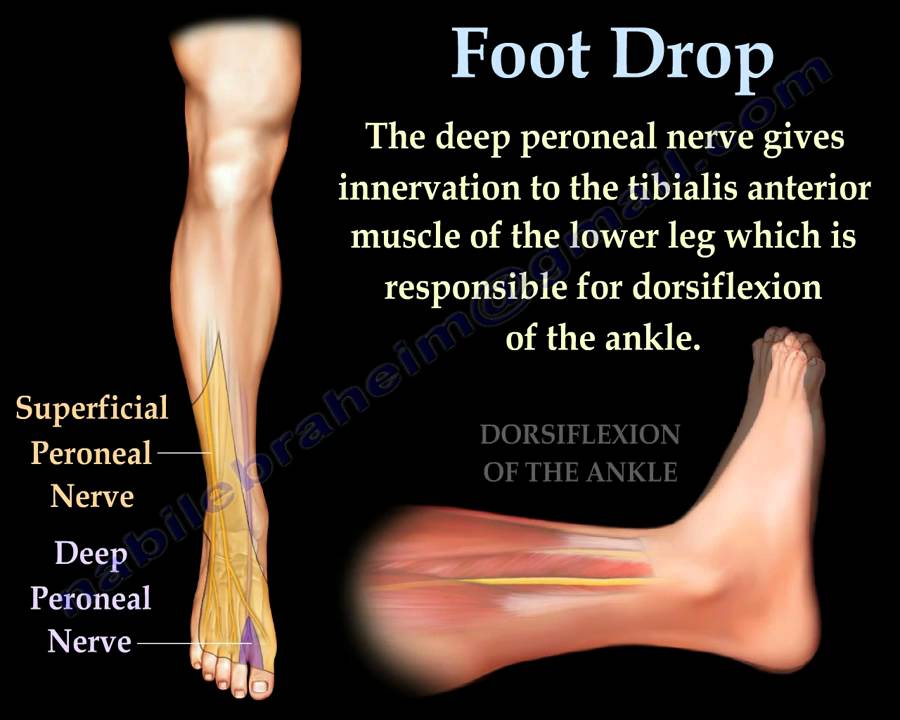
6. Weakness of dorsiflexors:
This produces foot slapping at early stance and foot drop at the swing phase. It is compensated by excessive flexion at the hip and knee (high stepping gait). When the hip flexors are too weak to perform hip flexion, the foot may be dragged forward with external rotation of the whole limb. Moderate weakness of dorsiflexors may not produce foot drop during the swing phase but may result in foot slap at heel strike. Mild weakness of the dorsiflexors will give rise to foot slap only during speedy walk or after the subject is tired.
7. Weakness of plantar flexors:
It results in dropping of the pelvis on the affected side with slowing of the forward movement at the terminal phase of stance phase. Speedy walking increases calf limp whereas it decreases during a gluteus medius limp. It must also be remembered that in gluteus medius limp, the pelvis on the side opposite to the affected limb is dropped as against the calf limp.
8. Antalgic gait:
In antalgic gait, due to the pain arising from ankle, foot, knee or hip, the stance period is reduced on the side of the painful leg. At the onset of the stance, the patient jerks his head, arms and trunk downwards; then with a jump and a long forward step leans towards the affected side and quickly shuffles the normal limb with a jump and a long forward step.

PHYSIOTHERAPY OF
GAIT TRAINING
It is important to note that gait training should be started after the first evaluation of a patient and not only when the patient is allowed to stand and walk. It consists of five phases:
1. Pregait training evaluation
2. Detection of the restricting factors
3. Therapeutic measures
4. Commencement of gait training
5. Independence in other activities of ambulation
1. Pregait training evaluation : evaluating the patient range of motion which is involved in ambulation with measurement of limb length.
strenghting and enduarance of of muscles participating in the ambulation.
2. Detection of the restricting factors
Proper interpretation of this data will help in detecting the possible restricting factors in gait and will also help in predicting the ultimate outcome.
3. Therapeutic measures
Appropriate therapeutic measures to correct or reduce the influence of restricting factors can be taken, e.g., correction of the soft-tissue contracture or deformity. It may be necessary to enhance strength, endurance and coordination to prepare the upper extremities to facilitate the use of a walking aid which may be required in future.
4. Commencement of gait training
The commencement of gait training will depend upon any of the following conditions of the patient:
(a) Non ambulatory phase
(b) Ambulatory phase
(c) Special training sessions to teach other advanced activities in ambulation
Non ambulatory phase
The mode of gait training will depend on whether the patient needs non–weight-bearing or partial weight-bearing ambulation. The patient may need total or partial support of the assistive device. During non–weight-bearing ambulation, the gait is nowhere near normal and the patient manages only by hopping on two crutches. But, at times the programme of conditioning the non–weight-bearing leg for future gait training needs more emphasis than crutch walking.

Ambulatory phase
A careful correlation of the deviations in gait in relation to actual deficiencies as noted earlier should be established. The end result of optimal expected correction in the gait training should be planned and begun.
Important factor to gait training is the education of the patient to normalize the abnormal attitudes by selfcorrection and encouragement. The ultimate goal is the normal to near normal pattern of gait which is safe and effortless.
If any compensation in length or orthotic device or walking aid is necessary, it should be given before starting gait training. On the spot correction with the patient made to practise in front of a postural mirror over the footmarks marked on the floor provides an excellent mean of gait training.


The usual physiotherapy techniques are practised to provide sound static and dynamic balance and stability to the gait; improving efficiency of gait along with training sessions for adopting the functional positions.
Reciprocal arm swinging provides opposite reaction forces. Arm movements in conjugation with pelvis and trunk rotation offer the necessary balance as well as symmetry to the gait. This forms a very important component of gait training. Unfortunately, this aspect is not given enough attention in our clinical programmes of gait training. This arm swing is basically a reflex action and if prevented, the upper trunk tends to rotate in the same direction as the pelvis, causing tense and awkward gait.
Judicious application of various physiotherapy gait training techniques supported by appropriate assistive devices and orthotic and prosthetic appliances can contribute potentially towards the improvement of the stability and gait pattern.
PNF techniques of resistive gait (pelvic resistance) with approximation at heel strike and rhythmic stabilization are very


effective for any gait training programme (Voss & Knott, 1968). Long sessions of standing balance on the affected leg alone are very effective to give confidence in improving the stability and the pattern of gait.
5.Independence in other activities of ambulation
Gait training cannot be considered complete unless the patient learns other ambulatory activities. Guidance and graded techniques of controlled resistance are very useful in providing independence in the following ambulatory activities:
1. Back walks
2. Turning
3. Side walks
4. Managing steps
5. Negotiating rough, uneven surfaces and slopes
6. Falling on the floor and raising Several sessions of practice and efforts are needed to achieve proficiency in these tasks. The metabolic cost of walking increases significantly in patients with lower extremity deficiencies resulting in early fatigue.


Impressive work .keep up the good work!!
ReplyDeleteYour knowledge is very good. Keep writing more
ReplyDelete